'This legislation reflects our commitment to patients and health care transparency, and I'm proud to see the progress we've made to better protect Hoosiers when they need it most.'
Gov. Eric Holcomb ceremonially signed into law legislation authored by State Rep. Brad Barrett (R-Richmond) to stop Hoosier patients from receiving surprise bills after out-of-network ambulance rides.
Barrett said individuals can receive large ambulance bills because the service provider was not covered by their insurance. Barrett authored House Enrolled Act 1385 to require health insurance companies to reimburse for ambulance services that are not part of a person's coverage plan.
"Ambulance services are critical to all Hoosiers but when insurance rejects a claim, patients are stuck with a huge balance," said Barrett, who serves as chair of the House Public Health Committee. "This legislation reflects our commitment to patients and health care transparency, and I'm proud to see the progress we've made to better protect Hoosiers when they need it most."
The new law also allows for out-of-network ambulance providers to receive payments from health insurance operators at locally set rates or at a capped rate based on Medicare benchmarks. Before, there was no set time frame in which an ambulance service must receive payment from health plan providers. Under this new law, service providers must receive payment within 30 days of the claim being filed.
For more information on House Enrolled Act 1385, visit iga.in.gov.

 Bill abolishing court positions passes Senate, Pulaski County could lose judge
Bill abolishing court positions passes Senate, Pulaski County could lose judge
 Detached garage fire damages home in Rochester
Detached garage fire damages home in Rochester
 Jonesy's Junction voted best tenderloin in Indiana
Jonesy's Junction voted best tenderloin in Indiana
 City council to consider food truck ordinance
City council to consider food truck ordinance
 ISP: Stay alert and share the road with farm equipment this spring
ISP: Stay alert and share the road with farm equipment this spring
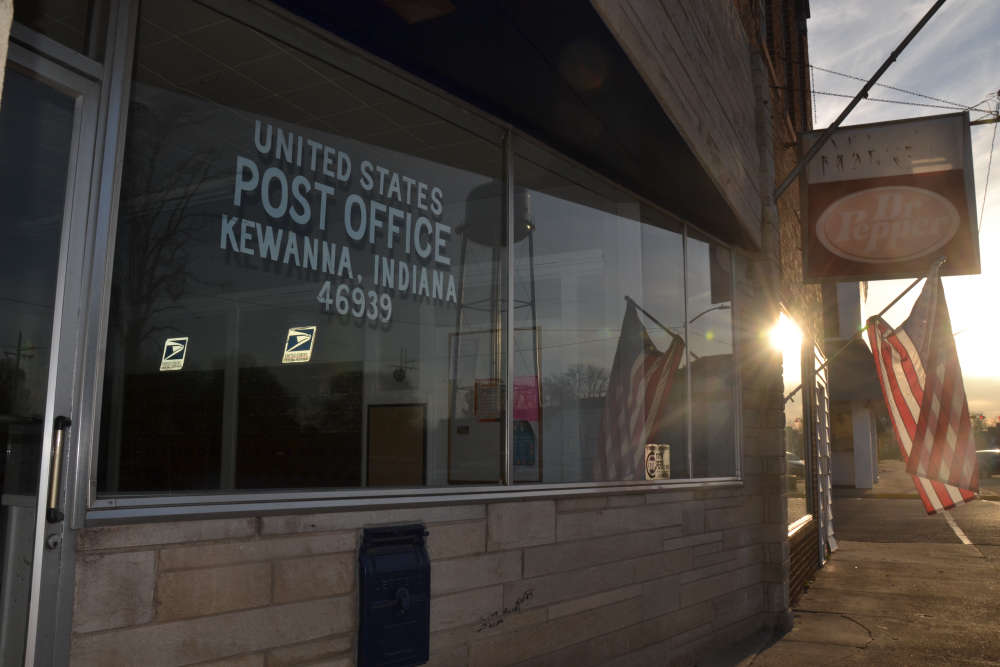 Kewanna residents gather to share frustration over lack of mail delivery
Kewanna residents gather to share frustration over lack of mail delivery
 Restaurants host fundraisers for local suicide prevention task force
Restaurants host fundraisers for local suicide prevention task force
 Bookings and Blotter – April 17, 2025
Bookings and Blotter – April 17, 2025