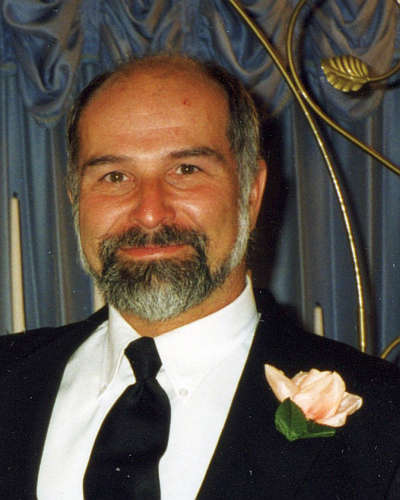
Attorney General Todd Rokita Friday announced a $700,000 settlement on behalf of Hoosiers to address allegations that a Hammond orthopedic surgeon overbilled Indiana’s Medicaid program.
“The purpose of Medicaid is to help patients in need cover health care expenses they otherwise would find difficult to pay,” Attorney General Rokita said. “The program is not intended to serve as a cash cow for providers.”
An investigation by Attorney General Rokita’s Medicaid Fraud Control Unit uncovered abnormalities in charges billed to Medicaid by the Southeastern Medical Center (SEMC), operated by Dr. Kishan Chand.
Between Jan. 1, 2016, and June 1, 2021, SEMC submitted approximately 13,101 claims indicating that medical staff performed spinal manipulation on patients who were under anesthesia.
Records, however, showed no associated billing for an anesthesiologist or a hospital or surgical center and that the frequency of billing by SEMC was a substantial outlier across all Medicaid providers — all of which raised the question of whether manipulation under anesthesia had been performed at all.
“Physicians and other providers have an ethical and legal obligation to accurately report medical procedures for which they seek Medicaid reimbursement,” Attorney General Rokita said. “My office will continue to ensure citizens’ tax dollars are protected from fraud and abuse by vigorously pursuing providers who have been unjustly enriched through improper billing.”
The Indiana Medicaid Fraud Control Unit receives 75 percent of its funding from the U.S. Department of Health and Human Services under a federal grant. The remaining 25 percent is funded by the State of Indiana.
Article provided by IN Attorney General's Office

 City Engineer details 2026 Community Crossing Matching Grant projects
City Engineer details 2026 Community Crossing Matching Grant projects
 Garbison sentenced to DOC on level 2 felony drug charges
Garbison sentenced to DOC on level 2 felony drug charges
 Kats sentenced to DOC for level 3 aggravated battery on infant daughter
Kats sentenced to DOC for level 3 aggravated battery on infant daughter
 New pavement markings to help drivers on northbound South Michigan Street at Pennsylvania Avenue
New pavement markings to help drivers on northbound South Michigan Street at Pennsylvania Avenue
 Rochester man charged with four felonies for crash causing death of Amish couple in June
Rochester man charged with four felonies for crash causing death of Amish couple in June
 Mobile Food Pantry in Bourbon Thursday
Mobile Food Pantry in Bourbon Thursday
 Blessing in a Backpack returns for Plymouth schools
Blessing in a Backpack returns for Plymouth schools
 Visit Fort Wayne releases annual list of Fort Wayne's "Best Spooky Halloween Displays"
Visit Fort Wayne releases annual list of Fort Wayne's "Best Spooky Halloween Displays"