.png)
community-health-network-agrees-to-pay-345-million-to-settle-alleged-false-claims-act-violations
Community Health Network, Inc. (Community), a healthcare network headquartered in Indianapolis, Indiana, has agreed to pay the United States $345 million to resolve allegations that it violated the False Claims Act by knowingly submitting claims to Medicare for services that were referred in violation of the Stark Law.
The Stark Law seeks to safeguard the integrity of the Medicare program by prohibiting a hospital frombilling for certain services referred by physicians with whom the hospital has a financial relationship unless that relationship satisfies one of the law’s statutory or regulatory exceptions. Under the Stark Law, when a hospital employs a physician, the hospital may not submit claims for certain services referred by that physician unless the physician’s compensation is consistent with fair market value and not based on the value or volume of their referrals to the hospital. In this lawsuit, the United States alleged that the compensation Community paid to its cardiologists, cardiothoracic surgeons, vascular surgeons, neurosurgeons, and breast surgeons was well above fair market value, that Community awarded bonuses to physicians that were tied to the number of their referrals, and that Community submitted claims to Medicare for services that resulted from these unlawful referrals.
The United States’ complaint alleged that beginning in 2008 and 2009, senior management at Community embarked on an illegal scheme to recruit physicians for employment for the purpose of capturing their lucrative “downstream referrals.” Community successfully recruited hundreds of local physicians, including cardiovascular specialists, neurosurgeons, and breast surgeons, by paying them salaries that were significantly higher – sometimes as much as double – what they were receiving in their own private practices. Community was well aware of the Stark Law requirements that the compensation
of employed physicians had to be fair market value and could not take into account the volume of referrals. Community hired a valuation firm to analyze the compensation it proposed paying to its recruited specialists. The Complaint alleged that Community knowingly provided the firm with false
compensation figures so that the firm would render a favorable opinion. The Complaint further alleged that Community ignored repeated warnings from the valuation firm regarding the legal perils of overcompensating its physicians. In addition to paying specialists excessive compensation, the Complaint alleged that Community awarded incentive compensation to physicians, in the form of certain
financial performance bonuses that were based on the physicians reaching a target of referrals to Community’s network, again in violation of the Stark Law.
“The Stark Law was enacted to ensure that the clinical judgment of physicians is not corrupted by improper financial incentives,” said Principal Deputy Assistant Attorney General Brian M. Boynton, head of the Justice Department’s Civil Division. “Today’s recovery demonstrates the Department’s resolve to protect the integrity of federal health care programs and to safeguard the taxpayer dollars used
to support these important programs.”
“Hoosier Medicare patients deserve to know that their care is based on their medical needs, not their doctor’s financial gain. When doctors refer patients for CT scans, mammograms, or any other medical service, those patients should know the doctor is putting their medical interests first and not their profit margins,” said Zachary A. Myers, U.S. Attorney for the Southern District of Indiana. “The United States alleged that Community Health Network overpaid its doctors, and that it paid doctors bonuses based on the amount of extra money the hospital was able to bill Medicare through doctor referrals. Such compensation arrangements erode patient trust and incentivize unnecessary medical services that waste
taxpayer dollars. The U.S. Attorney’s Office’s Civil Division, working alongside the U.S. Department of Health and Human Services Office of Inspector General (HHS-OIG) and the Justice Department’s Fraud Section are committed to holding companies accountable when they knowingly seek to profit off of Medicare patients through greedy compensation schemes.”
“HHS-OIG remains steadfast in our efforts to protect our health care programs and the people they serve, including holding those accountable who violate the Stark Law,” said Deputy Inspector General for Investigations Christian J. Schrank of the U.S. Department of Health and Human Services Office of Inspector General (HHS-OIG). “Our work will not cease here. Following the settlement, HHS-OIG
will enter into a five-year Corporate Integrity Agreement with the defendant, further demonstrating our unwavering commitment to protecting federal health care programs.”
Under the settlement, in addition to paying the United States $345 million, Community will enter into a five-year Corporate Integrity Agreement with the Office of Inspector General for the Department of Health and Human Services.
The settlement announced today stems from a whistleblower complaint filed in 2014 by CHN’s former Chief Financial and Chief Operating Officer, Thomas Fischer, pursuant to the False Claims Act’s qui tam provisions, which permit private persons to bring a lawsuit on behalf of the government and to
share in any recovery.
The Act also permits the Government to intervene and take over the lawsuit, as
it did in this case as to certain of Fischer’s allegations. Mr. Fischer’s share has not yet been determined in this matter.
The United States’ intervention and settlement in this matter illustrates the government’s emphasis on combating healthcare fraud. One of the most powerful tools in this effort is the False Claims Act. Tips and complaints from all sources about potential fraud, waste, abuse, and mismanagement, can be
reported to the Department of Health and Human Services, at 800-HHS-TIPS (800-447-8477).
The matter was handled by trial attorneys Arthur Di Dio, Kelly McAuliffe, Claire Horrell, and David Finkelstein of the Civil Division’s Fraud Section and Assistant U.S. Attorneys Justin Olson and Shelese Woods, from the Southern District of Indiana. The litigation team received investigative support from
the Federal Bureau of Investigation and the Department of Health and Human Services, Office of the Inspector General.
The case is captioned United States and the State of Indiana ex rel. Thomas Fischer v. Community Health Network, Inc., et al., No. 1:14-cv-1215 (S.D. Ind.). The claims resolved by this settlement are allegations only and there has been no determination of liability.

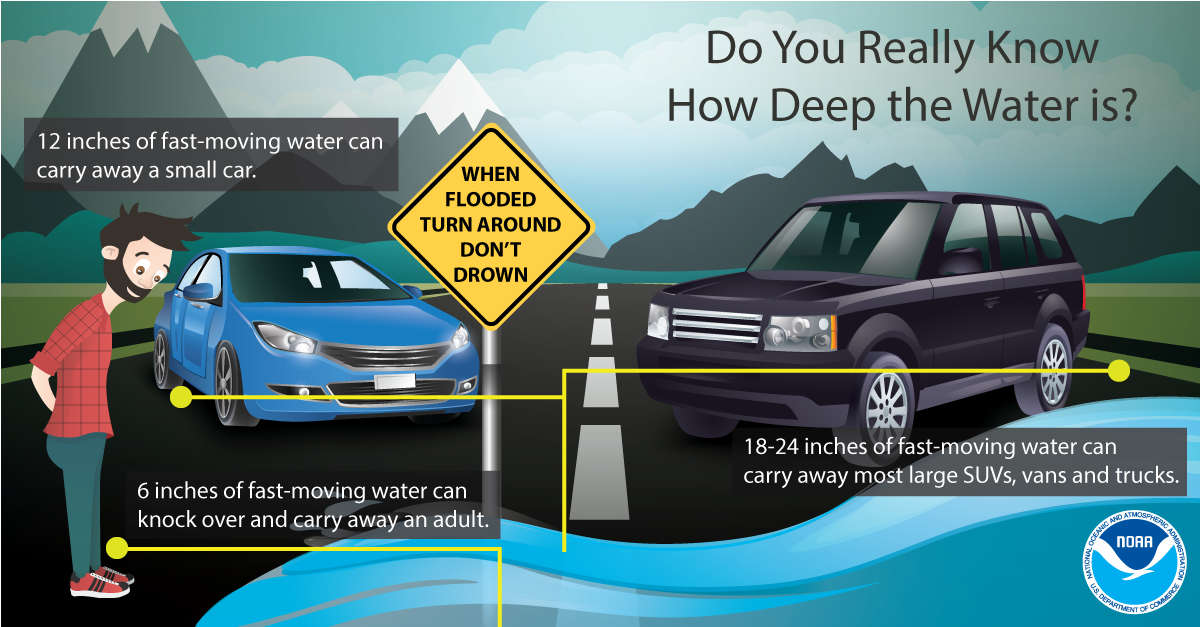 Flood Warning continues with more rain in weekend forecast
Flood Warning continues with more rain in weekend forecast
 Indiana State Parks hiring for lifeguards at public pools and beaches
Indiana State Parks hiring for lifeguards at public pools and beaches
 IDVA offers grant opportunities for non-profit organizations serving the Indiana Veteran Community
IDVA offers grant opportunities for non-profit organizations serving the Indiana Veteran Community
 Gov. Braun activates Indiana National Guard to aid in storm recovery
Gov. Braun activates Indiana National Guard to aid in storm recovery
 Passenger taken to IU-Methodist from two-vehicle Shelbyville crash
Passenger taken to IU-Methodist from two-vehicle Shelbyville crash
 Shelbyville makes major advancement in public safety and emergency response times
Shelbyville makes major advancement in public safety and emergency response times
 Registration open for Tree Trot 5K Run
Registration open for Tree Trot 5K Run
 Flat Rock Christian Church offers shelter Wednesday with potential severe weather
Flat Rock Christian Church offers shelter Wednesday with potential severe weather